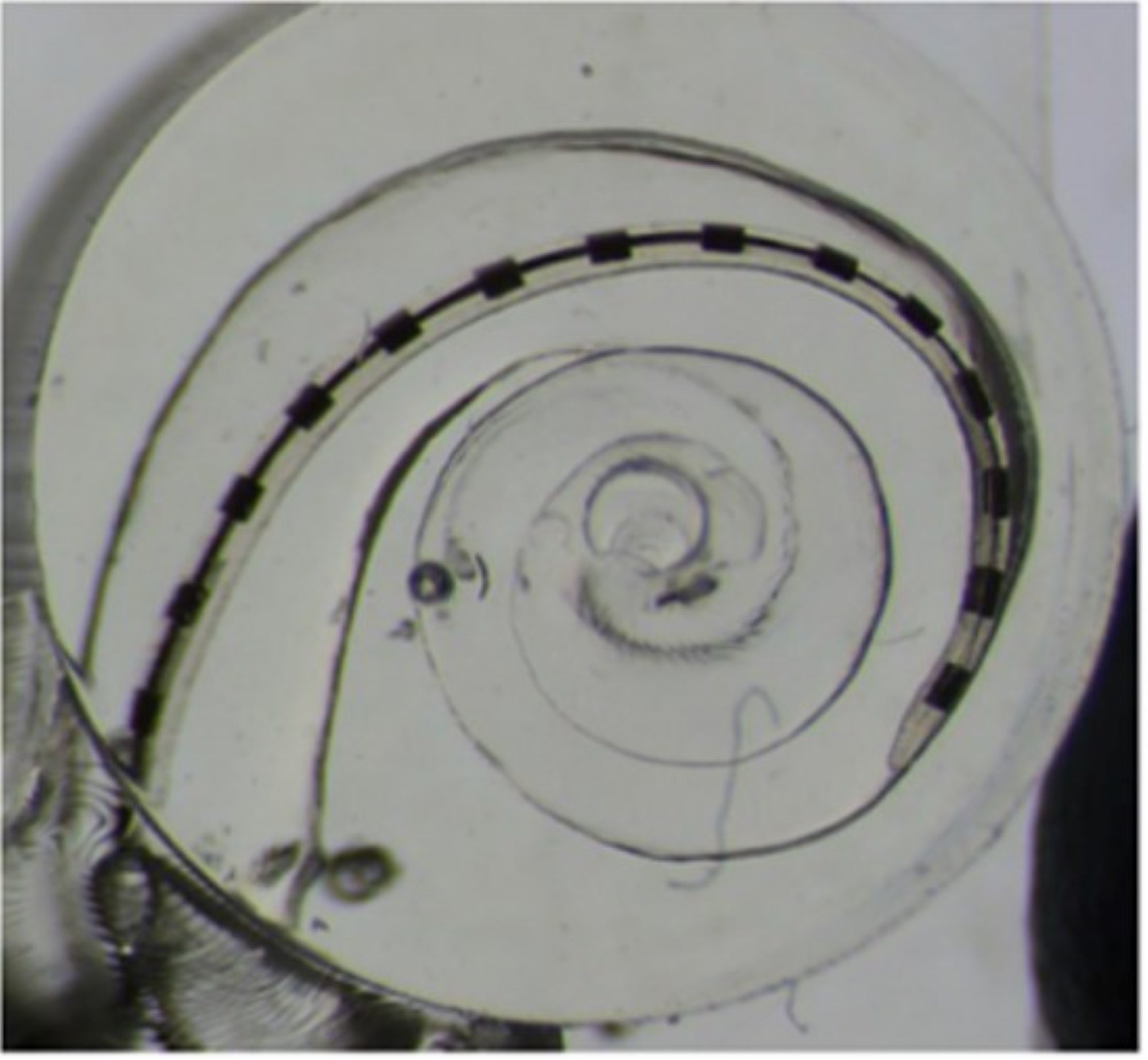
Physical Models
| By constructing anatomically accurate 3D printed models of the human cochleae, we can investigate the physical interactions of real cochlear implants with their environment. Mechanical models of the cochlea are crucial to understand the forces and resulting trauma that arise from cochlear implant insertion. Electrical models of the can replicate the dynamics and non-linearities of cochlear implant stimulation that are difficult to simulate computationally. Finally, fluidic models facilitate and understanding of the hydrostatic pressures that arise well as the injection of drug and gene therapy vectors as well as their distribution around the complex geometry of the cochlea. |
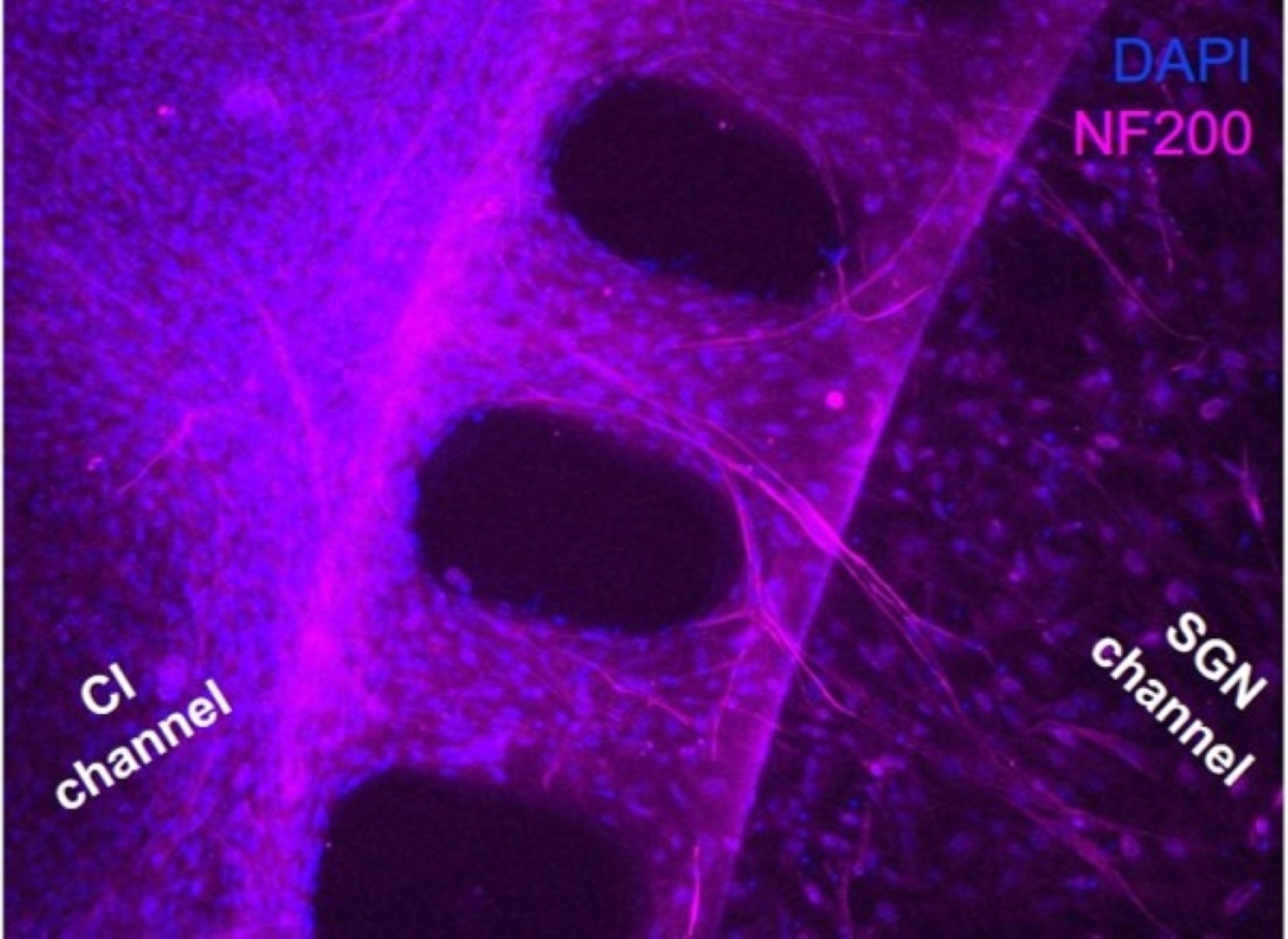
Cellular Models & Cochlea-on-a-chip
| In order to understand the electrode-neural interface that underpins the functionality of cochlear implants, we are leveraging a variety of electrophysiological techniques to understand auditory neuron responses to cochlear implant electrical stimulation. These range from patch clamp recordings of singular neurons to our "cochlea on a chip" microfluidic model which replicates the environment of the cochela and measures population neural activation with multi-electrode arrays. Inflammatory responses and fibrosis can also severely affect cochlear implant function therefore we have developed a tissue-engineered fibrotic cochlear implant model to investigate its effects. |
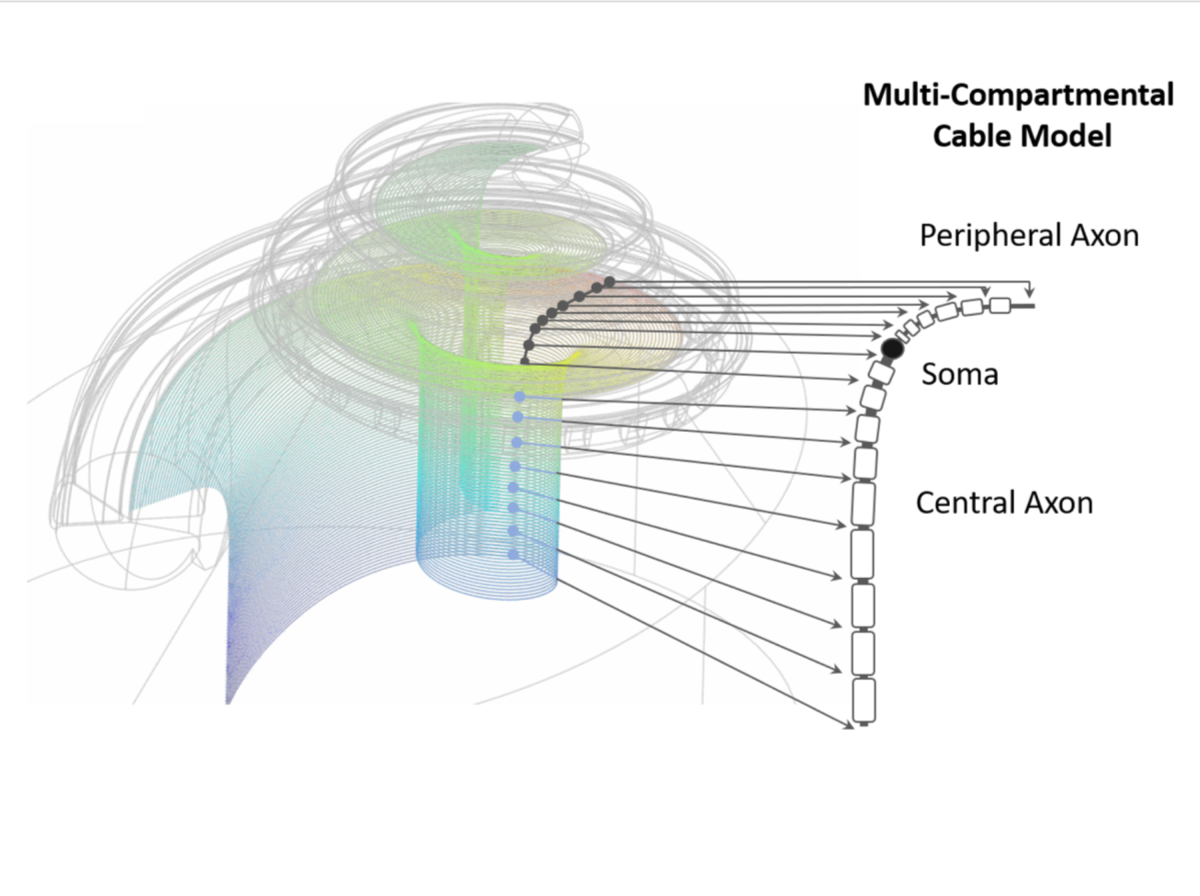
Computational Models
|
We are developed computational pipelines to both characterise the cochlear geometry and build models of the cochlear implant - neural interface. Through the combination of finite element modeling and machine learning, we have developed an end-to-end pipeline to predict speech outcomes in a range of simulated scenarios. By coupling these models with the experimental results from our parallel lines of research, we can build a complete picture to build accurate and validated predictive models that can accelerate the development of new techniques and technologies to improve patient outcomes. |
Development of Clinical Tools
| By validating our work in cadaveric specimens and in-patient measurements, we are developing clinical markers for a variety of scenarios that impair the use of cochlear implants. Our work ranges from the impact of extracochlear electrodes, facial nerve stimulation, and partial shorts within cochlear implants and their effects as well as tools to try and identify and inform clinical practice by providing more information on the state of the cochlear implant. |
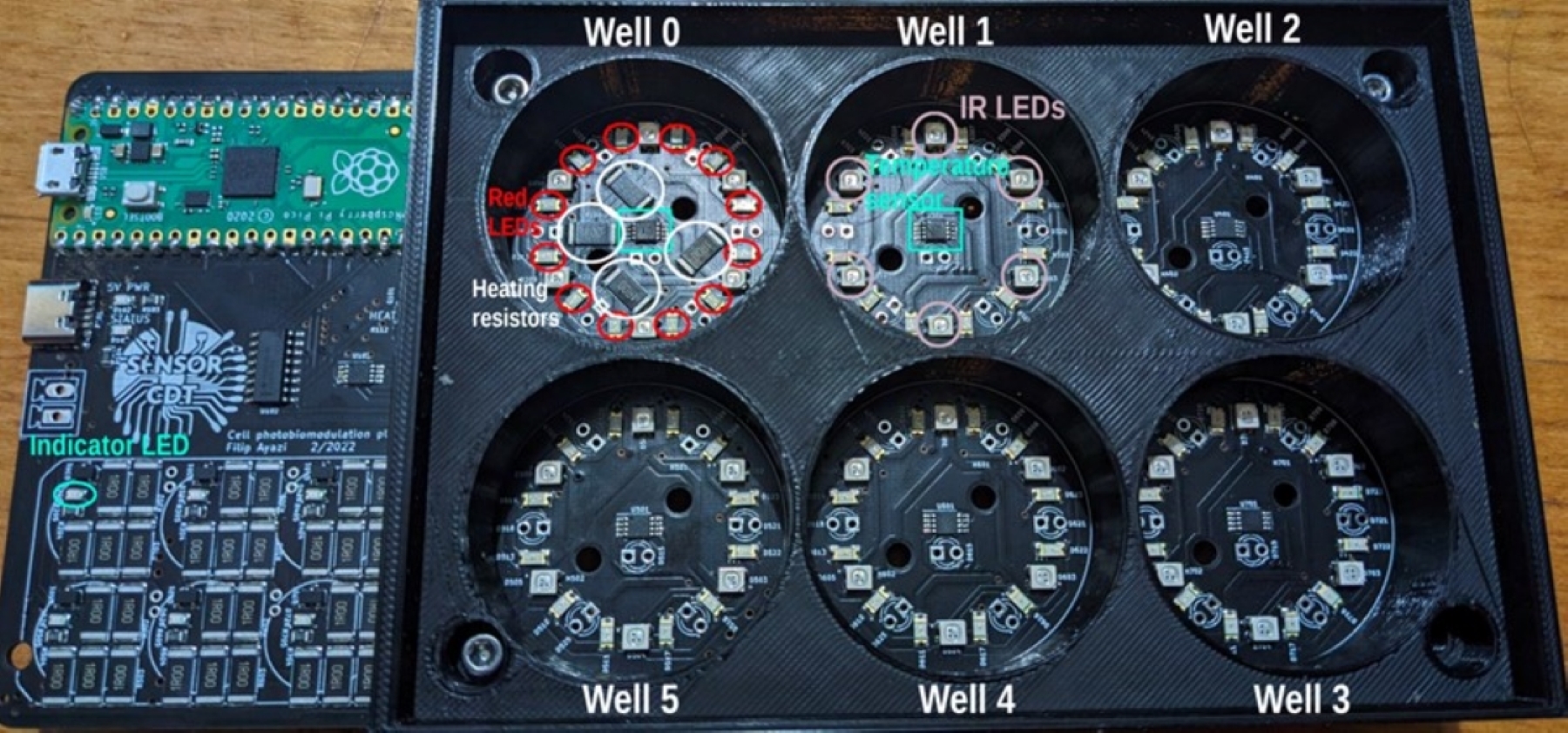
Photobiomodulation Therapy (PBMT) - with Dr. Gemma Bale, Engineering
| PBM uses near-infrared (NIR) is absorbed by Cytochrome Oxidate C, in the mitochondria, and affects cell metabolism and energy production. We are working on delivery mechanisms for this light to the inner ear, and testing its effects on cells in cell culture, and with patch clamping. We hope to protect against trauma from cochlear implants, ototoxic drugs, and noise using this non-contact non-invasive therapy. We are building computer models to predict power delivered to the inner ear, and generating prototypes for clinical use. |
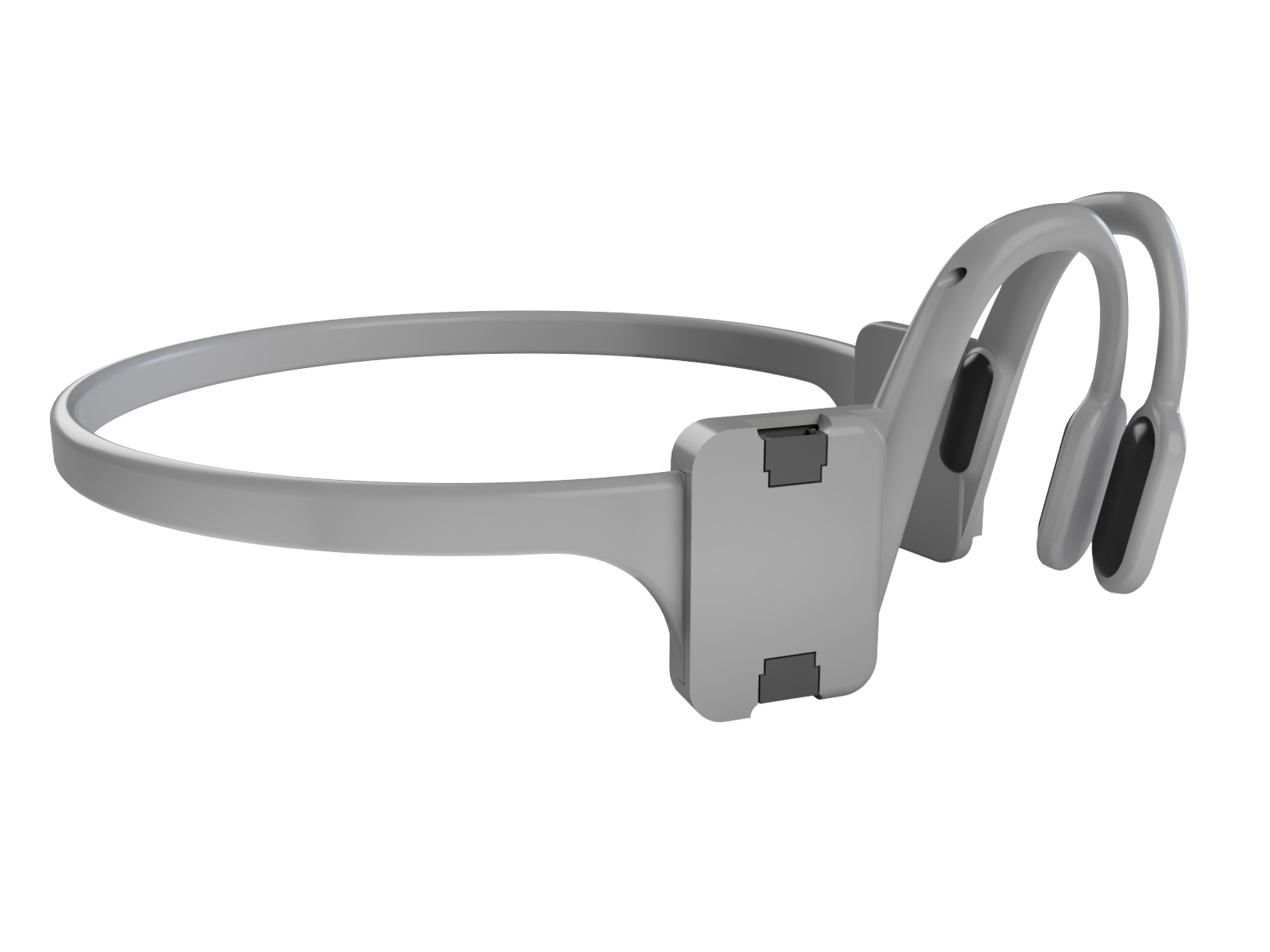
“Earables” with Prof. George Malliaras (Engineering) and Dr. Tom Stone (Human Locomotion Lab)
| We are interested in wearables that attach to the ear. Using these, we wish to measure EEG, head movements and eye movements. These can then be used monitor and diagnose disorders such as sleep disorders, epilepsy, neurodegenerative conditions and balance disorders. We are developing new EEG dry electrodes, new ear mountings, and new algorithms to achieve these aims. |